The lumbar spine is the low back. Spinal stenosis is a narrowing of the spinal canal, which contains the spinal cord and nerves (Fig. 1). This narrowing can put pressure on the spinal cord or on the nerves that branch out from the compressed areas.
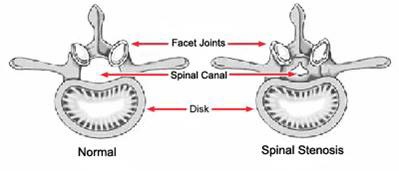
Fig. 1 Anatomy of the spine showing the spinal canal and the facet joints and disks.
Lumbar spinal stenosis most commonly causes cramping, pain or pins & needles in one’s legs; but it can also cause: back pain; loss of sensation in the legs; and sometimes problems with bladder or bowel function.


Spinal narrowing doesn’t always cause problems. But if the narrowed areas compress the spinal cord or spinal nerves, one is likely to develop symptoms. These often start gradually and grow worse over time. [1]
The most common spinal stenosis symptoms include:
Pain or cramping in the legs. Compressed nerves in the lumbar spine can lead to pain or cramping in the legs when one stands for long periods of time or walks. The discomfort usually eases on bending forward or sitting down, but it persists one continues to stand upright. Pain in the legs on walking is known as ‘claudication’ after the Roman Emperor Claudius, who had a limp. The form of claudication caused by lumbar spinal stenosis is called neurogenic claudication, because it caused by a problem with the nerves. Another type of claudication, vascular claudication, occurs when there is a narrowing or blockage in the arteries in the legs. Although both types of claudication cause similar symptoms, they differ in two important ways: vascular claudication usually becomes worse when one walks uphill and improves when one stands still. Neurogenic claudication is usually worse when going downhill and gets better when leaning forward or sitting down, because flexing the spine (bending forward) usually reduces the compression.
Radiating back and hip pain. Nerve compression can cause pain that starts in the hip or buttocks and extends down the back of the leg. The pain is worse when sitting and generally affects only one side (Fig. 2). Often this is referred to as ‘sciatica’ as the pain is largely in the distribution.
|
Fig. 2 Typical location of pain in sciatica. |
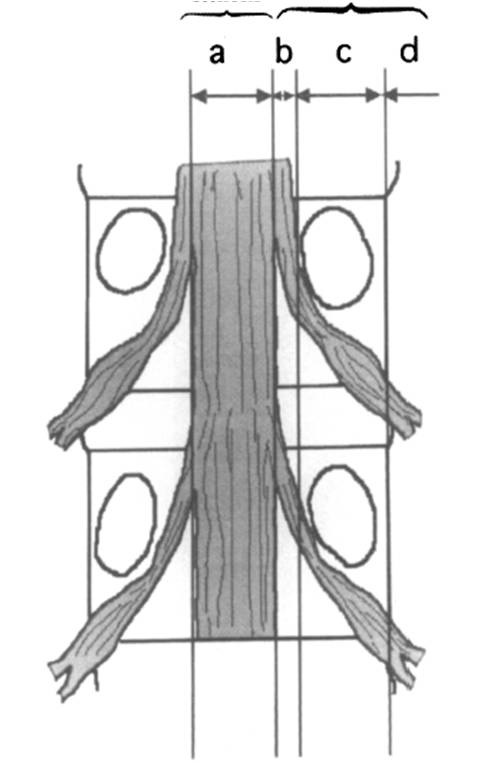
Fig. 3 Anatomical classification of lumbar spinal stenosis. |
Loss of bowel or bladder function (cauda equina syndrome). In severe cases, nerves to ones bladder or bowels may be affected, leading to partial or complete urinary or faecal incontinence.
If you experience these problems, seek medical care right away.
Are there different types of lumbar spinal stenosis?
Primary spinal stenosis, which is relatively uncommon, is present at birth.
Acquired spinal stenosis, which is the type that most people have, develops later in life. It’s usually a result of degenerative changes in the spine that occur with aging.
Anatomically, we can classify it into Central, Lateral, Foraminal, and Extraforaminal stenosis – this is relevant to treatment (Fig. 3). [1]
How serious is lumbar spinal stenosis?
Usually lumbar spinal stenosis only causes discomfort in the legs on walking, and it usually recovers completely with treatment, however, it can sometimes cause more severe problems, especially if treatment is delayed.
Permanent sensation loss. Lumbar spinal stenosis may cause a loss of feeling in one’s feet or legs. As a result, cuts or wounds may become seriously infected because one is not aware of them.
Loss of bowel or bladder function (Cauda equina syndrome). This complication is rather poor in prognosis. The recovery of the neurological deficit is unpredictable even after prompt surgical treatment.
Muscle wasting may be permanent, even after the pressure is relieved.


Lumbar spine degeneration is the most common cause.
Facet joint arthritis is osteoarthritis that affects the facet joints at the back of the spine. With time, the cartilage begins to deteriorate and its smooth surface becomes rough. If it wears down completely, bone may rub painfully on bone. In an attempt to repair the damage, the body may produce bony growths called ‘osteophytes’ or ‘bone spurs’. When these form on the facet joints in the spine, they narrow the spinal canal.
Herniated discs. These are also known as ‘slipped discs’. Herniated discs may occur on their own, or be one of the causes of spine stenosis. By the age of 30, the intervertebral discs may start to show signs of deterioration. They begin to lose their water content, becoming flatter and more brittle. Eventually, the tough, fibrous outer covering of the disk may develop tiny tears, causing the jelly-like substance in the disc’s centre to seep out (herniation or rupture). The herniated disc presses.
Ligamentum flavum hypertrophy. Ligaments in the back can undergo degenerative changes, becoming stiff and thick. The usual culprit in lumbar spinal stenosis is the ligamentum flavum (‘yellow ligament’) which runs inside the spinal canal. The thickening may press on the nerves, and the stiffening prevents the spine from moving properly.
Other Causes
There are other causes, such as spinal tumors, injury, Paget’s disease of bone, achondroplasia and others, but they are relatively uncommon and beyond the scope of this article.
What are the risk factors for lumbar spinal stenosis?
Age is the main risk factor for spinal stenosis. The risk of developing spinal stenosis increases after age 50. Other risk factors are a history of injury to the back, congenital stenosis, sports with overuse of the back muscles, and metabolic bone disease.
When should I seek medical advice?
Many people may ignore the early symptoms of spinal stenosis, believing that the pain and stiffness they experience are a normal part of aging. If pain, stiffness, numbness or weakness of the legs is troubling, it is appropriate to discuss the problem with a spine specialist. The rare complication of cauda equina syndrome warrants emergency surgical treatment.
How is lumbar spinal stenosis diagnosed?
History: The typical story is of pain in the legs with or without back pain.
Examination: Usually the back is stiff, but there are few other physical findings.
X-ray Lumbar Spine including views in flexion and extension. X-rays often show degenerative changes. They help to rule out problems that cause similar symptoms, including fractures, bone tumours, metabolic diseases etc. Flexion and extension views show if the spine is moving abnormally.
Magnetic Resonance Imaging (MRI). MRI uses a combination of magnetism and radio waves to produce three dimensional images. MRI is extremely useful for assessing the spine as it shows the nerves and other soft tissues as well as the bones. MRI produces cross-sectional images in three planes, allowing doctors to get a clear understanding of the anatomy. A special weight bearing MRI scanner which takes images with the individual standing up – this can be helpful, as lumbar spinal stenosis symptoms are usually only present when one is standing (Fig. 4). [2]
| Fig.4 The special weight bearing MRI scanner takes images with the individual’s positions | ||
|
A. Upright |
B. Tilting |
C. Supine |
Injection tests. Although the MRI produces beautiful pictures of the anatomy, it does not show ‘pain’. If one has back pain it is sometimes necessary to inject local anaesthetic into various places in the back to work out what is causing the pain.


Most patients are recommended non-operative treatment for at least 6 weeks. Surgical treatment will be advised if the patient is not responding well.
Physical therapy. Working with a therapist can build up the back muscle strength and endurance and improve the flexibility and stability of the spine. [3]
Rest or restricted activity. Moderate rest followed by a gradual return to activity may improve symptoms. Walking is usually the best exercise, especially for people with neurogenic claudication, but biking also is helpful because it keeps ones back in a flexed position, which reduces nerve compression.
A back brace or corset. This helps provide support and may especially benefit people who have weak abdominal muscles or degeneration in more than one area of the spine.
Paracetamol. Paracetamol/Acetaminophen (Panadol, Tylenol) is a mild analgesic, but has a synergy with other drugs. It is very safe when taken in the correct dosage, even in the long-term. If one is able to control ones pain with paracetamol it is probably not necessary to consider more aggressive treatment.
Non-Steroidal Anti-Inflammatory Drugs. These reduce inflammation and pain, but have the side effects of stomach ulcers and kidney damage. They include over-the-counter medications and prescription medicines which are generally stronger.
Some of the new ‘COX2 selective inhibitors" have all the advantages but few of the side effects of the older ‘non-selective’ drugs, and are very safe, even in long-term usage – though not quite as safe as paracetmol.
Narcotic Analgesics. A number of painkillers are effective but they often make one feel ‘woozy’ and one becomes tolerant to them in time, so they become less effective. They are best not used in the long-term.
Antidepressant and Antiepileptic Drugs. Many of them are very helpful for neuropathic pain. The common side effect is drowsiness (which can be helpful if the drugs are taken at night), but they can sometimes cause liver damage. [4]
Muscle relaxants. Some muscle relaxants are very helpful for back muscle spasm. They relax the muscles and have the synergistic effect with physiotherapy treatment. The major side effects are muscle weakness and drowsiness.
Chondroitin sulfate and glucosamine. These non-prescription food supplements, used either alone or in combination, reduce the pain of osteoarthritis, but not of nerve compression – so they may help back pain from facet joint arthritis, but they are unlikely to help leg problems. They are completely safe.
Epidural steroid injections. Steroids suppress inflammation and can be especially helpful in treating pain that radiates down the back of the leg. A single dose may provide significant relief. But because corticosteroids can cause a number of significant side effects, the number of injections one can receive is limited, usually to no more than three in one year. [5]


The goal of surgery is to relieve pressure on the spinal cord or nerves and to maintain the integrity and strength of the spine. This can be accomplished in several ways, depending on the cause of the problem. Broadly speaking, we can divide the surgical procedures into:
- posterior decompression alone
- posterior decompression with dynamic stabilisation
- posterior decompression with instrumented spinal fusion
Decompressive laminectomy
Indications: Decompressive laminectomy is for those with lumbar spinal stenosis with neurogenic claudication and/or sciatica pain but not back pain or a radiologically unstable spine.
Technique: This is the classic surgery for the lumbar spinal stenosis. By removing the entire lamina (the bone covering the back of the spinal canal), the nerves are decompressed. In conventional surgery, the surgeon makes a single incision in the back (Fig. 5). However, some surgeons do this procedure by a minimally invasive technique by using multiple small incisions. Although this takes longer, the patient usually has less pain and a faster rehabilitation.
 |
Fig. 5 Conventional incision for laminectomy. The muscles are retracted and the laminae are displayed. |
Risks: Complications are uncommon with modern techniques, but include infection, dural tear, nerve root injury, significant bleeding, deep vein thrombosis, paralytic ileus and neurological deterioration.
Results: Most people do extremely well with excellent relief of symptoms, but laminectomy does significantly alter the normal anatomy, potentially destabilising the spine. About 20-30% of the patients will need another surgery 5 years after laminectomy because of back pain, instability or recurrence of symptoms. At this stage, most of them will need a revision decompression and instrumented posterior spinal fusion (Fig. 6).
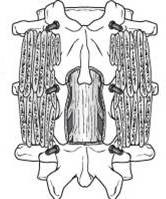 |
Fig. 6 Laminectomy and instrumented posterior fusion. The laminae have been removed to decompress the nerves. Three pairs of metal screws have been placed to hold the bone and bone graft has been placed to cause the two spinal segments to fuse together permanently. |
Laminotomy
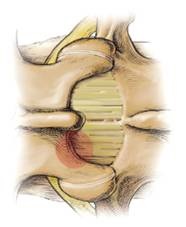
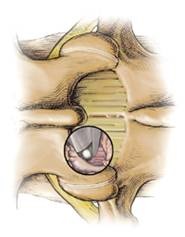
Indications: Decompressive laminotomy is for those with lumbar spinal stenosis with neurogenic claudication and/or sciatica pain but not back pain or a radiologically unstable spine. It is mainly indicated for spinal canal narrowing at the central and lateral recess. Only a small amount of tissue is removed (Fig. 7). The advantage is that one can preserve more the normal anatomy of the spine for the muscles to reattach. Theoretically laminotomy does not affect the stability of the spine as much as a laminectomy and with less chance of requiring a later fusion operation. This procedure can always be performed minimally invasively. [6]
| Fig. 7 Laminotomy | |
|
The shaded red circle shows the small area of the bone of the lamina and ligamentum flavum which is removed. |
The procedure can be performed minimally invasively – the black circle represents a tube through which special instruments are passed, thus requiring only a tiny incision. |
Technique: The surgeon removes only part of the lamina, bone spurs from the facet joint and thickened ligaments compressing on the dura or nerve roots. Risks: The risks are the same as for laminectomy.
Results: Most people do extremely well with excellent relief of symptoms.
Interspinous Process Distraction Devices
Indications: In milder to moderate cases of lumbar spinal stenosis, one may have spinal claudication with or without radiculopathy. If one’s symptoms are dynamic – in other words there is relief with bending forward - it is a good indication for insertion of an interspinous process distraction device (IPDD) (Fig. 8). The IPDD ‘jacks’ up the spine creating more space for the nerves.
 |
Fig. 8 An interspinous process distraction device sitting between the spinous processes at the back of the spine. |
Technique: This minimally invasive procedure performed via very small incisions. Sometimes laminotomies (see above) is performed at the same time. Usually one can get out of bed on the same day of the procedure.
Risks: Complications are uncommon with IPDD, because the device does not enter the spinal canal, but include infection, deep vein thrombosis, paralytic ileus and neurological deterioration. If laminotomy is performed at the same time, complications are the same as for laminectomy.
Results: Although IPDD is very new, results are encouraging so far. For moderate lumbar spinal stenosis, wide laminotomies and partial facetectomy is often performed in order to ensure adequate decompression. However, this may destabilise the spine in a way similar to conventional laminectomy. We believe that interspinous process distraction devices may stabilise the spine without the need for later fusion. [7, 8]
Posterior Instrumented Spinal Fusion
Indications: Severe lumbar spinal stenosis requiring extensive decompression; coexisting instability; severe deformity; associated back pain. Before the surgery, one may need discography and nerve root block to identify the origin of the symptoms. There is evidence showing that injection tests can provide useful advance indications of the likely success of the surgery.
Technique: The surgeon aims to realign the spine to a normal position, stabilise the spine to protect the nerves, and to treat the back pain. This procedure is composed of two parts. The first part is posterior decompression and the second part is spinal fusion with pedicle screws and bone grafting.
Mini-open or percutaneous Transforaminal Lumbar Interbody Fusion (TLIF) (Fig. 9) can be performed in the majority of the cases. The advantage is less bleeding, less wound pain, and faster rehabilitation than a conventional open spinal decompression and fusion. Normally, one would need to stay on bed for 2-3 days and be home within a week. Usually one is fully recovered and able to expected to resume full activity and sports at 6 - 9 months (the time for the bone to fuse).
 |
Fig. 9 TLIF The intervertebral disc has been replaced with a metal spacer and pairs of screws have been joined by robs to hold the bones without movement. Bone graft (not shown) is placed to cause the two spinal segments to fuse together permanently. |
Risks: The risks of surgery are the same as for laminectomy with the addition of implant malposition, failure of fusion, and accelerated disc degeneration at the adjacent segments. [9]


We can’t always prevent age-related changes in our backs, but the following steps can help keep our spine and joints as healthy as possible:
Exercise regularly. This helps maintain strength and flexibility in our spine, joints and ligaments. For the best results, combine aerobic activities such as walking and biking with weight training and stretching. Toning and stretching before exercise can help reduce wear and tear on the back. It also reduces the risk of injury by warming up muscles and increasing flexibility. Strength training can make the arms, legs and abdominal muscles stronger, which takes stress off the back. Start out exercise gradually and increase the duration and intensity of the workout
as we become stronger. Aim for at least 30 minutes of moderate exercise on most days.
Use good body mechanics. Being conscious of how we sit, stand, lift heavy objects and even how we sleep can go a long way toward keeping our back healthy.
Choose a seat that supports the lower back to minimise stress. If necessary, place a pillow or a rolled towel in the small of the back to maintain its normal curve.
When you drive, adjust the seat to keep both knees and hips level, and move the seat forward to avoid overreaching for the pedals.
Before lift something heavy, decide where to place it and how to get there. Pushing is safer than pulling. Always bend the knees so that both arms are level with the object. Avoid lifting overhead.
For the best sleep posture, choose a firm mattress. Use pillows for support, but don’t use one that forces your neck up at a severe angle.
Maintain a healthy weight. Extra weight puts additional stress on our bones and joints.
All Rights Reserved. Web Design by YSD