Introduction
Degenerative adult scoliosis (Fig. 1) occurs when the combination of age and deterioration of the spine leads to the development of a scoliosis curve in the spine. Degenerative scoliosis begins after the age of 40. In older patients, particularly women, it is also often related to osteoporosis. The osteoporosis weakens the bone making the bone more likely to collapse and causing further deformity. The combination of these changes causes the spine to lose its ability to maintain a normal shape. The spine begins to "sag" and as the condition progresses, a scoliotic curve can slowly develop.

Fig 1. X-ray of Degenerative Lumbar Scoliosis


When scoliosis occurs (or is discovered) after puberty, the condition is called "adult scoliosis". Adult scoliosis can be the result of untreated or unrecognised childhood scoliosis, or it can actually arise during adulthood. The causes of scoliosis that begins in adulthood are usually very different from those of childhood scoliosis. It is usually caused by other spinal conditions include degeneration, osteoporosis (loss of bone mass), post injury or even after previous spinal surgeries.


Degenerative adult scoliosis usually begins as low back pain. Small proportional of patient came to see their spine surgeon because of progressive spinal deformity. Since the degenerative process developed slowly, most of the patients have already adapted the symptoms. The symptoms are usually mild at the beginning until there is some complications happen to make the pain more severe to them. A combination of the degeneration of the spine and scoliosis deformity may cause pressure on nerves and possibly even the entire spinal cord. This can lead to weakness, numbness, and pain in the lower extremities. In severe cases, pressure on the spinal cord itself may cause loss of coordination in the muscles of the legs making it difficult to walk normally.


Medical History
In order to make a proper diagnosis and rule out other possible conditions, the first step is to take a medical history such as the primary symptoms of the lower back, the history of the deformity of the lower back, functional loss affecting the daily living, any family history of scoliosis, neurological symptoms include muscle weakness, sensation loss and spinster dysfunction. Previous history of any spine surgery and other medical conditions are crucial for the decision of the treatment.
Physical examination
We start with general assessment such as gait assessment, posture on standing (Fig. 2), and bending movement of the body. This give us a general idea of how severe is problem affecting their daily lives. Specific examinations include measurement of the leg length, measuring the rib hump, flexibility of the curves, any lower limb neurological dysfunction. Occasionally, we will need to check the sphincter functions by digital rectal examination.

Fig 2. Kyphotic deformity associated with scoliosis


After the examination, X-rays will be ordered that allow us to see the structure of the spine and measure the curves. Basic X-rays include standing whole spine AP and Lateral view (Fig 3). Motion lateral views of the lumbar spine in flexion/extension are important. These pictures provide us a gross idea of how severe of the deformity and at the range of motion of the spine. Supine side bending AP views are also necessary to look at the reducibility of the curve if surgery is considered. Measured Curve Progression is usually done by comparing the X-rays taken at different stage. Any past X-rays taken of your spine can be very helpful to your spine surgeon.

Fig 3. X-ray Whole Spine AP/LAT on standing
MRI scan (Fig. 4) lumbar spine is required to look for any spinal cord compression or nerve root compression. Spinal stenosis is the most commonest associated pathology leading to pain and/or lower limb neurological symptoms. It is the commonest reason to bring the patient to the spine surgeon.

Fig 4. Typical MRI scan findings in Degenerative Scoliosis patients
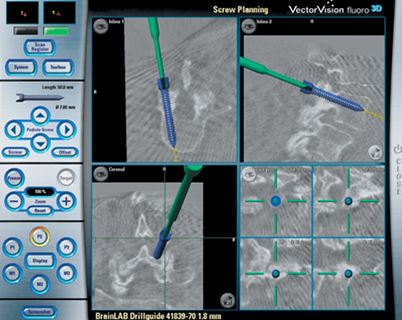
Fig 5. CT Guided Navigation for Pedicle Screws Insertion
Computerised Tomogram (CT) scan (Fig.5) is also useful for the assessment. By reconstructing the images, we can see the deformity in 3D way. The data from CT scan can also be used in navigation machine to guide us the direction of the screw fixation during the surgery.


The treatment for degenerative scoliosis is usually start with non-surgical at the beginning. It includes: medications, exercise, and certain types of braces to support the spine. Mild pain medications may be recommended for use when needed. Strong pain medications, such as narcotics, are not recommended due to the risk of addiction.


Oral anti-inflammatory and neuropathic pain medications (e.g. Gabapentin, Pre-garbalin) are adjunct to the pain medications to control the arthritis symptoms and nerve pain. If osteoporosis is present, then treatment of the osteoporosis may slow the progression of the scoliosis as well. This can be accomplished in several ways. The current recommendations include weight-bearing exercises, Calcium and vitamin D supplement, Hormone replacement therapy, and Bisphosphonate (Fosamax, Actonel), Bonviva, and Para-thyroid hormone injection (Forteo).


It is commonly prescribed to patients with back pain due to degenerative lumbar scoliosis. It helps to relief the back pain and stiffness. Core muscle strengthening may reduce the progress of the symptoms but not the speed of the progress of the degeneration or deformity.


The use of a spinal brace may provide some pain relief. However, in adults, it will not cause the spine to straighten. Once you have reached skeletal maturity, bracing is used for pain relief rather than prevention. If there is a difference in the length of your legs, special shoe inserts or a simple shoe lift may reduce your back pain.


Surgery is usually recommended when the scoliosis become severe and painful. Surgery to relieve pain due to scoliosis is a controversial topic. However, if the pain is chronic and debilitating, it is an option that can be discussed with your doctor. Lower limb neurological symptoms such as numbness, claudication (limited walking distance) and nerve pain (radiculopathy) are strong indication for surgery. These symptoms are usually related to lumbar spinal stenosis. To learn more about lumbar spinal stenosis, please refer to FAQ’s of Lumbar Spinal Stenosis.


In principle, the options for surgery include decompression and spinal fusion with appropriate degree of correction of deformity. Decompression is a term that means remove the pressure on the nerves or spinal cord (Fig. 6). Usually this means reducing or removing part of the bony structure in the lumbar spine such as a degenerated disc or bone spur. The procedure is called laminotomies or laminectomies. This procedure can be done via minimal invasive technique with small incision at around 2 cm or less. In one level surgery, it usually takes 1.5 hour to complete with 50 cc or less blood loss. The recovery time is around 2-3 weeks.
Fig 6. Endoscopic Posterior Decompression for Spinal Stenosis
If the deformity is severe or the spinal segment is not stable after decompression, fusion (connecting 2 vertebrae together) is indicated. There are many techniques in performing lumbar spinal fusion. Recently there is a new technology specifically benefit the degenerative lumbar scoliosis, called Direct Lumbar Interbody Fusion (DLIF) and Oblique Lumbar Interbody Fusion (OLIF) (Fig. 7 & 8). Basically these two spinal fusion techniques are very similar. They are using small incision from the left side of the abdomen to achieve correction of the scoliosis and fusing the unstable spinal segment. By distracting the lumbar disc, indirect decompression of the foramen and central spinal canal can be achieved. In addition to the posterior screws fixation, decompression via laminotomies or laminectomy can provide further decompression if the indirect decompression is still not enough. These procedures are also a minimal invasive type of surgery with blood loss at around 100-200 cc. With the help of neuro-monitoring, the chance of neurological complication is extremely small. Recovery is much faster and easier than the previous surgical techniques.
In conclusion, long survival in our society is inevitably producing more age related health issue. As we are more healthy and physically active, we encountered more degenerative lumbar scoliosis. It is a very major surgical challenge both the patients and the spine surgery. With the advance of technology, now we can treat this kind of pathology with much easier way. The surgical outcome and risk of the treatment is much improved.
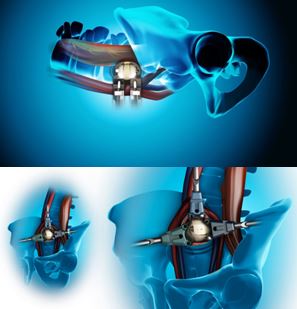
Fig 7. Oblique Lumbar Interbody Fusion (OLIF)
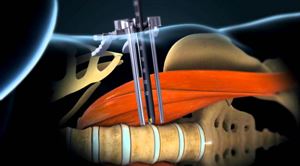
Fig 8. Direct Lateral Lumbar Interbody Fusion or Extreme Lateral Lumbar Interbody Fusion (DLIF/XLIF)
All Rights Reserved. Web Design by YSD


